Tips for CYP feeding or eating disorders
Who is this for?
These tips have been developed for professionals working across health care; from primary and universal care to hospital general paediatric services through to specialist Child and Young People Mental Health Services (CYPMHS).
Introduction
This is the first of four tip sheets to provide you with quick access learning on feeding or eating disorders in children and young people. Infants 0-2 years are covered in a fifth, separate tip sheet.
Feeding or eating disorders (FEDS) are complex, and potentially life-threatening mental illnesses that can affect anyone regardless of age, gender, ethnicity, sex, socioeconomic group or background. There are many myths and misconceptions surrounding eating disorders combined with a lack of knowledge. This can produce many negative outcomes such as preventing someone from reaching out for help.
This first set of tips is divided into four sections (A-D), and aims to support you in raising your awareness and earlier recognition.
Section A - Be aware
Section B - Know the diagnostic categories
Section C - Be aware of what works in treatment
Section D - Understanding the origins of feeding and eating disorders
Section A - Be aware
Stigma and blame are impediments to early detection and good care
Don’t be afraid of starting the conversation about people’s relationships with food
Feeding or eating disorders are easily missed: so be alert because early intervention leads to better outcomes
- The earlier someone is able to access treatment or support for their eating disorder, the greater chance they have of making a full and sustained recovery
- Eating and feeding disorder symptoms may be obscured due to apparent social norms e.g. vigorous exercise in someone overweight, restricting certain food types, weight loss in someone who is overweight…look out for compulsive unhealthy or extremes of behaviour including in normal weight young people
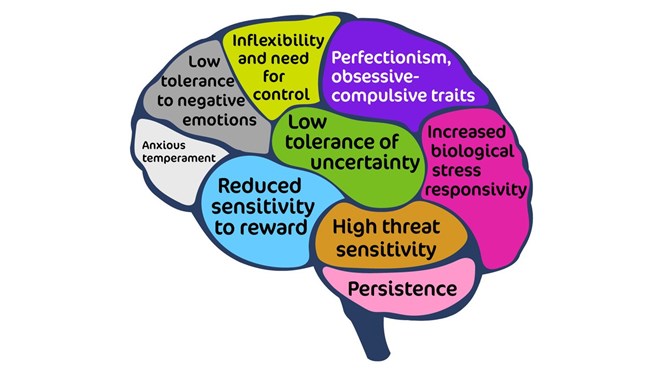
- Look at the slide and think about the risk factors listed that contribute to the development of eating disorders
- Beware of outward appearance. It may not always be obvious that someone has an eating disorder, nor does someone have to be underweight to be suffering with an eating disorder
- Be alert and know the person may be very unwell, much more so than they may first appear. For example, check their weight and rate of weight loss, their blood pressure, their ECG, blood biochemistry, haematology and nutritional status (refer to what to look out for tips)
Remember that feeding or eating disorders are mind-body conditions, care must be holistic to be effective
- Beware of focussing only on the psychological and missing the physical or vice versa, support must include both
- There is no one single cause and each person will present slightly differently and may not have all the recognised symptoms for one eating disorder
- For treatment, you must look at each person as an individual and address both the physical and psychological impact
Feeding or eating disorders affect all ages, sex, gender, race and ethnic groups
- Feeding or eating disorders may occur at any age, of any ethnicity, gender or background
- Anorexia nervosa most often emerges in mid-adolescence and somewhat later bulimia nervosa
- Regardless of age (childhood, early, mid or late adolescence, young adults) the emerging condition may well interrupt emotional and social development. This can complicate the recovery process during treatment.
Earlier intervention matters: detect and refer early
- Anorexia nervosa has one of the highest mortality rates for any mental illness
- Death can result from suicide (20%), Heart/ECG related events, low potassium levels, chronic low albumin levels, long term illness, malnutrition
- However, early detection makes all the difference
- NICE guidelines 2017 say that
- Full recovery is possible.
- The sooner someone gets the treatment they need, the more likely they are to make a fast and sustained recovery.
- A ‘wait and see’ attitude with young people who are developing an eating disorder is not usually helpful.
- The sooner someone with an eating disorder starts an evidence-based NICE-concordant treatment the better the outcome.
- NHS England recommended access and wait times standards for evidence-based treatment to be started are:
- a maximum of 4 weeks from referral with a designated healthcare professional for routine cases
- Within 1 week for urgent cases
- In cases of emergency, the eating disorder service should be contacted to provide support within 24 hours
- Be sure you get blood biochemistry, haematology and ECG results on the same day to ensure rapid and safe clinical decision making for young people who are severely restricting food and rapidly losing weight or who are engaging in multiple daily episodes of vomiting and/or laxative abuse
- Initially appointments should be weekly and should include weighing of the patient, especially for people who are restricting their food intake (for example in anorexia nervosa, ARFID and rumination regurgitation disorders, but also sometimes OFSED and bulimia nervosa
Aim to work with the family
- Eating disorders affect the entire family, therefore family members play an integral role in treatment and should be involved regardless of the patient’s age, although the way they are involved may differ for older adolescents
- Family is a great resource to support good outcomes, mobilise strengths and build collaboration. Including the young person in finding solutions together
Early psychoeducation is important for the young person, their family and carers
- Young people with feeding or eating disorders may feel increased anxiety around mealtimes
- People with restrictive feeding or eating disorders may feel more anxious/agitated/distressed/guilty before, during and after eating, and less anxious when they don’t eat
- People who binge eat might experience temporary relief from challenging emotions and thoughts like a sense of emptiness when bingeing, but distress and shame may return afterwards
Positive outcomes are expected for the majority of young people with feeding or eating disorders
- By the end of treatment, 50-75% of children and adolescents with anorexia nervosa are in remission and at long term (7 years follow-up), only around 10% will have a diagnosis of an eating disorder. Less than 15% will directly transition from child and adolescent, to adult services. Around one third of young people who had treatment as children and adolescents will have additional treatment for their eating disorder as young adults
- For bulimia nervosa we can expect over 50% will do well and be free from the symptoms
- For ARFID we don’t know – there are no comparable longitudinal studies at this stage
- Comorbidity, most often with anxiety and/or depressive disorder, is common in children and adolescents with an eating or feeding disorder and this needs to be addressed and treated as well
Be aware young people with feeding or eating disorders may lack insight into their condition or being unwilling to talk about it
- Young people with anorexia nervosa & other FEDs might have great difficulty in seeing how unwell they are or may be in denial about their illness.
- Despite having full clarity of thought and reasoning in their world, outside their feeding or eating disorder
- However, the multidisciplinary team should focus on ensuring that the patient's health and safety have to come first
- It is important to note that many people with bulimia nervosa, binge eating disorder, ARFID have struggled with disordered eating and distress for many years before seeking help
There are many effects of starvation
Below is a short list, further information is provided in our Tip Sheet 2 What to look out for.
- Low mood
- Stress hormones increase - cortisol goes up
- Sexual hormone levels are reduced; amenorrhea is one consequence in females
- A negative cycle of effects on thinking and feeling occurs that make the eating disturbance worse
- physiological effects such as delayed gastric emptying, which means the young person feels full quicker, even though the body is malnourised
- and multiple other physical effects please refer to what to look out for tips
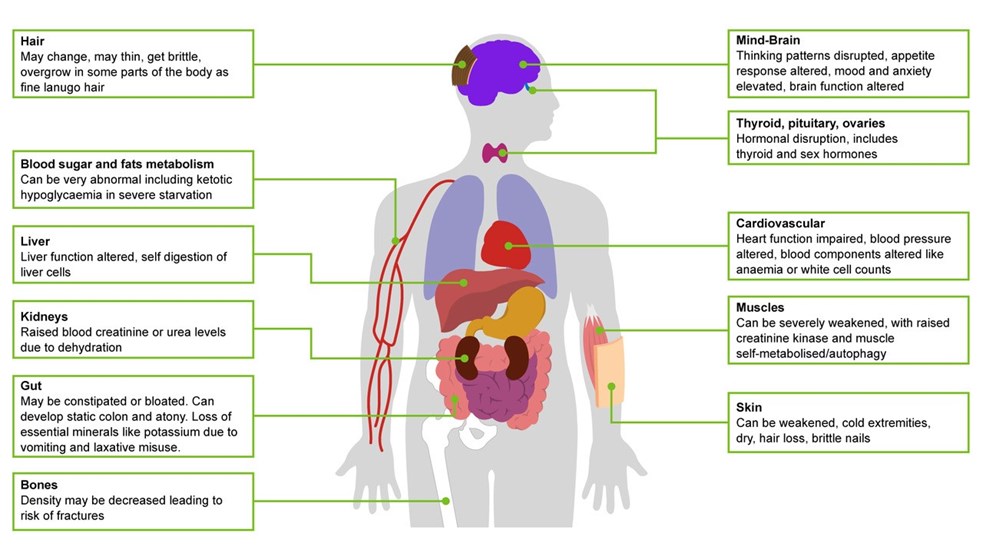
- Osteopenia (thinning of bones)
- Starvation increases the drive to eat in some people, and can trigger binge eating behaviour
Section B - Know the diagnostic categories
There are seven specified types of feeding or eating disorders (ICD11): be familiar with them so you don’t miss them
- Anorexia nervosa
- Bulimia nervosa
- ARFID: Avoidant restrictive food intake disorder
- Binge eating disorder
- Rumination - regurgitation disorder (RD)
- Pica
- Other specified feeding or eating disorders (OSFED)
- This includes purging disorder (without bingeing). Be aware this can occur in people with type 1 diabetes, when insulin omission is used to influence weight. This is known as Type 1 diabetes and eating disorders (for more information see resources including MEEDS guidance)
- An eighth category in ICD11 is for ‘unspecified feeding or eating disorders’ (FEDU)
- For more on each type of disorder see our tips on what to look out for
One important distinction between different FEDs is whether body image distortion/dissatisfaction is directly linked to the eating disturbance
- Body image distortion/dissatisfaction is a core driver of AN/BN
- For other FEDS like binge eating disorder and related OSFED presentations, it is sometimes present but not the main issue
Section C - Be aware of what works in treatment
Tip sheet 4 'What to do' provides much more detail on interventions
The best treatment for ARFID will depend on the specific issues underlying the eating disturbance in the individual
Bulimia also has severe physical consequences: regular eating breaks the cycle of bingeing and starving
BED, ARFID, RD and pica can also have severe physical consequences. Just different ones
Increase food intake to establish steady gradual weight gain: address starvation as the best first step for anorexia nervosa
- This may also be required in rumination-regurgitation disorder and ARFID
Weight matters for health but is a poor measure of health on its own and differs between people
- In young people, weight, height and BMI need to be adjusted for age and gender using growth charts. They are important indicators of health but NOT the only measure of physical risk.
- Use the published guidance on Medical Emergencies in Eating Disorders (2022) to perform a comprehensive assessment of risk
The illness drives the thinking, it’s not a simple choice for the person
- The brain consequences to altered food intake include increased anxiety and distress when eating
- Increasingly entrenched habits and patterns occur with more rigid thinking and reluctance to ‘try new things out’, which runs counter to normal adolescent development
What do young people say they want from professionals?
- I want to receive collaborative, person-centred treatment that is focused on my needs and not just my weight or BMI (body mass index), to help me recover mentally as well as physically.
- I want professionals to show compassion, understanding and trust, while not making assumptions based on my diagnosis.
- Professionals who are working with me will understand how feeding or eating disorders can affect people differently, and how they might get in the way of people accepting help.
- I want people involved in my care to communicate with me and be open and transparent, explaining why certain decisions are made. I want to be able to voice my opinion and to be fully informed throughout my treatment.
Section D - Understand the origins of feeding & eating disorders
Key factors
- Some occur long before the onset of a feeding or eating disorder, some are close to onset and are triggers, and some maintain the problems once started
Risk factors
- Risk factors can be biological, psychological, social-cultural context and media related, developmental-neurodevelopmental, for example:
- Predisposing factors: genes, family history of eating disorder, addiction, mood disorders, diabetes, personality traits, low self-worth, relationship problems, overvaluation of shape, weight and food, difficulty managing emotions, sport activities like marathon running or ballet, brain changes being identified in studies, having a family member with eating disorder, higher weight, social media, rigidity of thinking (AN), risk avoidance (AN), perfectionism (AN and somewhat BN), low self-esteem (all), general anxiety (all), 50% of AN people have an anxiety disorder
- Triggers: stressful life events and losses - the pandemic may turn out to be one of these too, traumas, including all forms of abuse, food allergies and or coeliac disease, sport activities, other people’s comments about weight or shape, social media, advertising of ‘ideal’ body imagery.
Further Information
Resources
BEAT-HEE-RCPsych
- BEAT Tips Poster
- BEAT leaftlet: Seeking treatment for an eating disorder? The first step is a GP appointment.
- BEAT carers booklet: Eating disorders: a guide for friends and family
- Type 1 diabetes with an eating disorder: more information
- BEAT elearning for nurses (for all ages, not child and young person specific - Each of the 3 sessions will take around 30 to 60 minutes to complete and includes additional learning resources for those looking to further increase their knowledge. To access the elearning in the elfh Hub directly, please visit the links below.
Medical Emergencies in Eating Disorders (MEED)
- Medical Emergencies in Eating Disorders (MEED). Guidance on recognition and management. RCPsych College Report CR233, May 2022. (Replacing MARSIPAN and Junior MARSIPAN)
- Guidance on Recognising and Managing Medical Emergencies in Eating Disorders. Annexe 1: Summary sheets for assessing and managing patients with severe eating disorders. RCPsych College Report CR233, May 2022. (Replacing MARSIPAN and Junior MARSIPAN)
- Medical Emergencies in Eating Disorders. Annexe 2: What our National Survey found about local implementation of MARSIPAN recommendations. RCPsych College Report CR233, May 2022. (Replacing MARSIPAN and Junior MARSIPAN)
- Guidance on Recognising and Managing Medical Emergencies in Eating Disorders. Annexe 3: Type 1 diabetes and eating disorders (TIDE). RCPsych College Report CR233, May 2022. (Replacing MARSIPAN and Junior MARSIPAN)
NHSEI, NICE, NCCMH
- Eating Disorders: Recognition and Treatment NICE Guideline (NG69) 2020
- Access and Waiting Time Standard for Children and Young People with an Eating Disorder: Commissioning Guide, particularly in relation to managing transitions between services 2015
- Eating Disorders Quality Standard (QS175) 2018
- NHS England children and young people’s eating disorders programme 2019
References
- Bould H, De Stavola B, Lewis G, Micali N. Do disordered eating behaviours in girls vary by school characteristics? A UK cohort study. Eur Child Adolesc Psychiatry 2018; 27: 1473–81.
- Byford S, Petkova H, Stuart R, Nicholls D, Simic M, Ford T, Macdonald G, Gowers S, Roberts S, Barrett B, Kelly J, Kelly G, Livingstone N, Joshi K, Smith H, Eisler I. Alternative community-based models of care for young people with anorexia nervosa: the CostED national surveillance study. Southampton (UK): NIHR Journals Library; 2019.
- House J, Schmidt U, Craig M et al. Comparison of specialist and non-specialist care pathways for adolescents with anorexia nervosa and related eating disorders. Int J Eat Disord 2012;45:949-956
- McClelland, J., Simic, M., Schmidt, U., Koskina, A., & Stewart, C. (2020). Defining and predicting service utilisation in young adulthood following childhood treatment of an eating disorder. BJPsych Open, 6(3), E37
- Neale J, Pais SMA, Nicholls D, Chapman S, Hudson LD. What Are the Effects of Restrictive Eating Disorders on Growth and Puberty and Are Effects Permanent? A Systematic Review and Meta-Analysis.J Adolesc Health. 2019 Nov 23. doi: 10.1016/j.jadohealth.2019.08.032.
- NICE guideline (NG69) 2017. Eating Disorders; recognition and treatments.
- Nicholls D, Becker A. Food for Thought: Bringing Eating Disorders out of the shadows. BJPsych 2019 Jul 26:1-2.
- Petkova H, Ford T, Nicholls D, Stuart R, Livingstone N, Kelly G, Simic M, Eisler I, Gowers S, Macdonald G, Barrett B, Byford S. Incidence of anorexia nervosa in young people in the UK and Ireland: a national surveillance study. BMJ Open 2019; BMJ Open 2019 Oct 22;9(10)
- Simic, M., Stewart, C.S., Konstantellou, A. et al. From efficacy to effectiveness: child and adolescent eating disorder treatments in the real world (part 1)—treatment course and outcomes. J Eat Disord 10, 27 (2022)
- Stewart, C.S., Baudinet, J., Munuve, A. et al. From efficacy to effectiveness: child and adolescent eating disorder treatments in the real world (Part 2): 7-year follow-up. J Eat Disord 10, 14 (2022)
- Vanessa Huke, Jeremy Turk, Saeideh Saeidi, Andy Kent, John. F. Morgan. Autism Spectrum Disorders in Eating Disorder Populations: A Systematic Review. European Eating Disorders Review. First published: 31 July 2013
Further elearning from NHS HEE & MindEd
Children and Young People - MindEd resources
1) Eating Disorders in Young People
Description: For General Health CYP Entry Level Audience (5-18 yrs)
This session gives an overview of the nature, aetiology and risk factors linked to eating disorders. Also covered are the diagnostic elements that allow us to distinguish between eating disorders and other conditions affecting the eating behaviour of young people.
Author(s):
Dasha Nicholls
2) Eating Disorders; Anorexia and Bulimia
Description: For Specialist Mental Health CYP Health Entry Level Audience (5-18 yrs)
This session is aimed at more experienced/specialist users and outlines the diagnostic criteria and non-specific risk factors for eating disorders that most often start in childhood and adolescence. The eating disorders most frequently seen by mental health professionals, for example, anorexia nervosa, are explained in more detail. Treatment interventions and treatment outcomes for anorexia nervosa and bulimia nervosa will be discussed, with particular emphasis given to the key family therapy interventions for anorexia nervosa.
Author(s):
Mima Simic
Description: For wider general health audience (0-5 yrs olds)
This session describes the normal developmental progress of children from birth to five; from breast/bottle to eating independently and the difficulties encountered by parents during this developmental process.
Author(s):
Judy More
Description: For Families/parents/carers, Universal Audience (about CYP 5-18 yrs)
This session gives parents basic information and advice about the eating disorders: anorexia nervosa, bulimia nervosa, binge eating and similar behaviour, that do not usually meet threshold criteria. It is not intended to address childhood obesity or infant eating difficulties.
Author(s):
Brian Jacobs
Mima Simic
5) Eating Disorders (CT): Families and Professionals
Description: Specialist CYP mental health entry level (5-18 yrs)
This session describes Community Eating Disorder Services for Children and Young people (CEDS-CYP) and the importance of accessing the right support for these disorders early. It explains the physical risks and psychological aspects of eating disorders and the multi-disciplinary nature of CEDS-CYP. It highlights the importance of engaging the young person in treatment and the role of the family in this. The session also outlines psychological and medical treatments, the need to attend to the often co-occurring psychiatric conditions and the use of medication.
Authors:
Mima Simic,
Rachel Bryant-Waugh
6) Eating Disorders (CT): Further Information for Professionals
Description: Specialist CYP mental health entry level (5-18 yrs)
This session will provide a background to Community Eating Disorder Services for Children and Young People (CEDS-CYP) and the assessment and treatment of eating disorders. It will cover psychological treatments, appropriate use of medication and co-occurring conditions.
Authors:
Mima Simic,
Rachel Bryant-Waugh
All ages - NHS HEE TEL Resources
Eating disorders training for health and care staff
This suite of training was developed in response to the Parliamentary and Health Service Ombudsman (PHSO) investigation into avoidable deaths from eating disorders, as outlined in recommendations from the report titled Ignoring the Alarms: How NHS Eating Disorder Services Are Failing Patients(PHSO, 2017).
It is designed to ensure that health and care staff are trained to understand, identify and respond appropriately when faced with a patient with a possible eating disorder. It is the result of collaboration between eating disorder charity Beat and Health Education England with key partners.
Eating disorders training for medical students and foundation doctors
This eating disorders training is designed for medical students and foundation doctors. The two sessions will take around 20-30 minutes to complete and includes additional learning resources for those looking to further increase their knowledge. The sessions also provide good preparation for those who go on to participate in medical simulation training on eating disorders.
Eating disorders training for nurses
This eating disorders training is designed for the nursing workforce. Each of the 3 sessions will take around 30 to 60 minutes to complete and includes additional learning resources for those looking to further increase their knowledge.
Eating disorders training for GPs and Primary care workforce
This eating disorders learning package is designed for GPs and other Primary Care clinicians. The two sessions will take around 30-40 minutes each to complete and includes additional learning resources for those looking to further increase their knowledge.
- GPs and Primary Care: Understanding Eating Disorders
- GPs and Primary Care: Assessing for Eating Disorders
Medical Monitoring in Eating Disorders learning for all healthcare staff who are involved in the physical assessment and monitoring of eating disorders
The eating disorders learning package for Medical Monitoring is designed for primary care teams, eating disorder teams or other teams who are monitoring the physical parameters of a person with an eating disorder. The session will take around 30 minutes to complete and includes additional learning resources for those looking to further increase their knowledge.
Acknowledgements
These tips have been curated, drawn and adapted from a range of existing learning, including MindEd, NHSei, NICE, MMEEDs guidance, NHS HEE elfh/BEAT/RCPsych resources. Extracts from the MMEEDs are included with permission courtesy of the MMEEDs team.
The content has been edited by Dr Mima Simic (MindEd CYP Eating Disorders Editor) and Dr Raphael Kelvin (MindEd Consortium Clinical Lead) with close support of the inner expert group of Prof Ivan Eisler, Dr Dasha Nicholls, Dr Rachel Bryant Waugh and Dr Simon Chapman.
A wider expert reference groups include BEAT (Kathrina Dixon-Ward, Martha Williams, Brooke Sharp), Dr Elaine Lockhart (RCPsych Child and Adolescent Faculty Executive chair), Gemma Trainor (MindEd Consortium RCN lead rep), Prof Ulrike Schmidt (Professor SLAM/KCL and MindEd Editor) Dr Lisa Shostack (MindEd Consortium BPS Lead Rep).
Disclaimer
This document provides general information and discussions about health and related subjects. The information and other content provided in this document, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment.
If you or any other person has a medical concern, you should consult with your healthcare provider or seek other professional medical treatment. Never disregard professional medical advice or delay in seeking it because of something that you have read in this document or in any linked materials. If you think you may have an emergency, call an appropriate source of help and support such as your doctor or emergency services immediately.
MindEd is created by a group of organisations and is funded by NHS England, the Department of Health and Social Care and the Department for Education.
© 2023 NHS England, MindEd Programme