Acknowledging loss and bereavement in education settings
 Created together with Education Support Partnership
Created together with Education Support Partnership
Acknowledging loss and bereavement in education settings
This set of tips from our international panel of experts and adapted for education staff are intended to help staff to:
- understand the impacts of loss and bereavement on themselves and colleagues
- use this understanding to respond with patience and compassion
- know that loss and bereavement are universal human experiences
- support their education setting as a place where staff can support each other through loss and bereavement, and in so doing build resilience together
There are two main sections; ‘things to do’ and ‘things to know’. Use this resource as works for you. The headline tips give rapid access advice, the drop downs beneath each tip provide more detail.
Introduction
Loss and bereavement are normal but can be very difficult events in life. There is no rule book for facing loss or managing the death of someone close to you. Bereavement is personal and each person has to find their own way to make sense of loss and death. However, the way others support us when we are bereaved can make a real difference to how we manage.
In our education settings, bereavements can impact from multiple domains of school life including:
- Pupils’/students’ bereavement from the loss of a family member/friend/teacher
- Staff experiencing bereavement of a family member/friend/colleague or following other major losses such as miscarriage of a pregnancy
- The death of a pupil/student within the school community
- The death of a member of staff within your school community
- For some staff and pupils alike, loss of a much-loved pet is also a significant bereavement
Bereavement
Within a school, the death of anyone connected to the school can impact on the whole community. The way adults behave in these circumstances can shape how everyone responds. It is a time to balance grief, strength, remembrance, respect, spirituality, faith, resilience, and kindness. Our words and our actions can have a wide impact in these moments. The social focus on grief and bereavement has heightened during the pandemic, affected by the media and social media. The media focus on death as a result of COVID-19 is not necessarily replicated in our education settings, where people in our communities continue to be affected by loss and the death of those they love and care for from diverse circumstances, illness, injury and tragedy. There is no good way to lose someone you love.
However, for many, the process of bereavement was interrupted during the pandemic. Some people have been unable to say goodbye to loved ones and grieve in their own way, across faiths, cultures and personal preferences. People may have had to grieve without the kind of support that they would normally have from extended family and friends. In some societies there is a lot of visiting of relatives and so if you have a colleague whose family is far away and has few nearby relatives, then they might need extra support from the school community. This all may have a longer-term impact.
Grief takes time, there are no set rules, and it differs from person to person. Don’t be surprised that people react very differently. Watchfully waiting, being alert to the signs of your own or another’s distress, and generally looking out for each other helps.
Loss without death
It is important to recognise that people can also suffer loss without death. You, or someone you are close to may experience:
- Family loss through separation: because of a relationship breakdown, divorce, or moving out of an area, including emigration
- Traumatic loss of a loved one: sudden brain injury, Alzheimer’s, dementia, or prolonged mental health crisis. In these scenarios you still see a loved one, but mourn the person you used to know
- Economic loss: due to changes in financial security through job loss, unemployment, or debt
- Loss of safety: where there is impact of domestic abuse, or because of a house break-in or assault
- Loss of trust: family member with an addiction, or betrayal
- The national response to the pandemic may also have created the loss of regular contact, loss of support with childcare or caring duties, loss of familiar routines, loss of usual ways of expressing spirituality, faith, or religion; loss of physical contact, loss of community, loss of hoped-for futures and opportunities
These tips don’t offer a right way to be, but they do suggest some strategies that may support you or those around you, at one of the most difficult periods of life. Whether it is you who is affected, or you are supporting others.
Things to do
These tips are written for your personal loss or bereavement, but they can all be adapted if you need to help others with their own grief.
Acknowledge and allow yourself your feelings and thoughts at times of loss
- It is normal to experience a wide range of feelings and thoughts: e.g. overwhelming sadness, happy to have had the person in your life, angry they have gone, cheated that you didn’t say goodbye. Some people may even experience relief or guilt which can be confusing, and may lead to the need for some more support from others... allow yourself to experience any or all of this, it’s not wrong in some way, it is just what it is for you
- You may find you are suddenly being hit by grief, by a connecting piece of music, smells, food or places that connect with the deceased
- You may be numb and not expressing feelings, but worried that others will think you heartless for not caring
- Balancing all these conflicting emotions can be exhausting
- It’s okay to share how you feel, but also okay not to share
It can help to find an image for your grief – this technique is called visualisation
- Some people describe grief as being like waves washing over them. These waves change their pattern over time, they are not linear... before the tide gradually recedes
- Allowing yourself to give in to the emotion flooding through you can, at times, be affirming
- Another image that reflects how grief changes over time might help some: grief is like a bouncy ball in a room that reduces in size over time. You do not know when it will hit you (larger and more frequent at the start) but it is different as the size of the ball reduces and bounces less
- By using a visual metaphor you can feel more in control of when those feelings take you, making it less likely you will feel overwhelmed by grief in the middle of your working day
- You can allow yourself these feelings when you feel safe and secure to do so
Developing a narrative to support your journey of grief or loss may be helpful
- You could develop a repeating story that helps to capture good memories relating to who or what you have lost. For example, through written narrative or in your mind, you could go to a cottage in the woods and as you enter each room, you will put in an object that holds a good memory
- You may want some help to guide your visualisation technique
- For some people, talking about memories with others is more helpful than spending time developing narratives and images in their own heads
- If you have few or no positive memories of the person, that can make it more complicated to work through your grief. Additional support may be needed from your family, faith group, community, friends and or professionals
Coping with the death of someone we care for is usually an emotional experience
- As time goes by, some feelings will support you to grieve and recover and other feelings will slow down your healing
- Don’t feel guilty if you laugh or enjoy yourself during a period of mourning
- Be respectful of how others may feel about grief, but don’t let them dictate how you should feel
- Be aware that feelings may be evoked in others when they hear of your grief, perhaps your loss becomes a trigger to remember their own grief. If you are grieving you may not have the emotional space left to support them too. Try to direct them kindly towards other avenues of support
- Your feelings are your own and you have reason to hold them, but if your feelings are mostly negative, after a period of time it may be important to seek some help. Suggested resources are listed at the end of this tip sheet
Feeling angry is normal, staying angry can be a problem for you and those around you
- Loss or bereavement can feel very lonely, even when we are doing some of the pushing away ourselves. This can lead to feelings of anger, and frustrated anger can cause us to push others further away. Break the cycle by accepting or giving a small act of kindness
- Communicate to others how you are feeling. Let them know you appreciate them, even if you can’t accept their help just yet. This may be in a text, a letter or send a message through a third party. No communication is isolating for those you care for as well as you
- Find a way to take part in physical activity, ideally with others, but even if you are on your own exercise can provide an outlet for feelings; physical activities can help emotional regulation and support a sense of agency and self-esteem
Actions you can take: memory making is important
- Treasure something that represents a fond memory of the person who has died
- Plant a flower they liked in a pot or garden
- Keep a photo on your laptop of a place they loved
- Choose a lovely shell or stone to keep in a pocket or a bag, so that each time you hold it you allow yourself a brief memory
- Memories which make you laugh are good too
- Writing a memory in the form of a letter or eulogy can be very supportive to you and those around you
- Plan for days which you know may be harder, such as birthdays, anniversaries or Christmas. It is okay if others have forgotten to mark those days – don’t judge them, each person copes in their own way
‘Coping too well’ is not a thing
- Be respectful of how others manage their loss or bereavement, even if that looks like they don’t care as much as you do. Remember the wave metaphor they may be in a different place in their waves
- We don’t know how others feel and how they may mourn quietly and privately
- Not everyone needs to mourn in public, or for long – it doesn’t mean they didn’t love
- Holding positive memories and a knowledge that you had had a good relationship can mean that you feel less need to mourn
- Covering up feelings is not the same as coping. Covered up feelings will need to be tackled at some point further down the line
There is no ‘good time’ to stop grieving: grief is not linear
- Grief is a natural process to help humans heal from loss or death
- It is okay to still think of those we have lost as often as we choose
- It is helpful to contain or hold those feelings, after a time of mourning, so that grief doesn’t prevent us living our best life
- It’s okay to let life begin to grow again around your grief
- If your grief continues to impact on your wellbeing, family life, relationships or ability to do your job, then you may need to seek some help. Suggested resources are listed at the end of this tip sheet
Grieving can be hard when you are surrounded by people and children with their own immediate needs in an education setting
- Allow yourself to be distracted by your work, but there will be moments when you are also distracted from your work. Speak with a colleague if this balance is not right for you or the children you are working with
- You may find grief overwhelms you at points. Build some strategies to help manage this, for example, keep a pebble in your pocket to hold when you need a moment to refocus
- Be aware of the lessons that are coming up. If the curriculum requires the class to learn about birth this may relate. to your own loss. You could try to change the order of the curriculum, or speak with your team leader about swapping with someone else for that set of lessons
- It may be important to you to share with the children what you are going through. It could be beneficial to rehearse what you want to say with a colleague first. Children are able to show real empathy, but it is important that they don’t take on your sadness as their own burden
You can expect the team in your education setting to support you at this time
- Your setting should have a policy that relates to leave in special circumstances, which has been advised by Trade Unions. If you don’t have one, or it hasn’t been updated for a while, this may be something that you could research or revise (see resources section)
- Having a ‘buddy’ or a colleague who will support you during your process of bereavement can make a big difference
- Not all education settings will have enough room for you to have a quiet space for reflection if you need it, so you may want to agree going offsite at break and lunchtimes for a few minutes to help you cope - either with or without a colleague
- You may find it helpful to talk to a senior manager about what you feel your needs will be whilst at school following a loss.
- If sitting in your car for five minutes at the start of the day is your ‘normal’ for a while, it will help others to know
- Remember, it can be really hard for colleagues to know how and when to support you at these times. They may need a bit of help in knowing what will be supportive
Take time to learn about bereavement and grief when you are not overwhelmed with such feelings yourself
- It helps to understand the usual range of moods, thoughts and feelings that can come with grief
- It can be important to know how loss and bereavement are supported by different religions and cultures
- Take time to consider how death and loss is approached in film and literature
Bereavement has often been complicated by the pandemic
- Bereavement has become complicated by the coronavirus pandemic.
- Education setting staff may have been impacted by the decisions about the care of sick relatives. For example:
- the stress of caring for relatives who are not, or who choose not to be admitted to a hospice/hospital at the end of their life. The whole family may have to shield etc.
- someone may have died at home, especially if this was unexpected
- Colleagues may have lost loved ones without the opportunity of spending time with them before and as they died. They may be experiencing:
- The pain of not being able to visit someone dying in hospital/hospice
- Fears about what happened to their relative when they were dying
- Family beliefs, traditions and religious rituals are likely to be very important for the whole family
- Families may not have been able to follow their expected rituals and traditions. This can add to the burden
- Not being able to say goodbye / view the body / attend funeral and other cultural rituals all affect children as well as adults in families
Things to know
Remember your own needs
Do
| Keep eating regular meals, exercise, even if only a brisk walk, and maintain sleep routines (even if you can’t sleep well) | |
| Secure a safe emotional anchor for yourself; the people and beliefs that are central to you are important at times like this. This may be your faith, community, partner, family, friends; things that give meaning and stability to your world | |
|
Seek help if you aren’t coping |
|
| Hold a good memory in your mind, keep up your social contacts. Reflect on positives in your relationships at work and at home |
|
| Be kind to yourself Seek training and information about loss and bereavement |
|
| Remember 5 Rs to support wellbeing and build resilience | |

Don't
- Give yourself unrealistic timeframes to ‘feel better’
- Dwell on what you could have said or done
- Close the door to those who may be a good support to you when you are ready
- Inadvertently superimpose your views and feelings on those you are supporting
- Feel rejected if a person you are supporting isn’t ready to talk. Be available for whenever they do want to do so
For some colleagues, loss is made more complex by other characteristics or vulnerabilities, such as;
- Previous traumatic loss, or abuse
- Caring responsibilities
- A race, culture or faith that is not shared by others
- Restrictions to usual religious or faith-based rituals, curbed by the pandemic
- Lack of acceptance, or rejection by family members
- Ongoing family physical or psychiatric illness
- Physical vulnerabilities
- Mental health difficulties
- Hidden disabilities
Some warning signs that a person may need extra help
- Ongoing sadness or depression, with a reduced interest in daily activities. This may vary during the day; there may even be moments of pleasure and joy but the main mood is sadness
- Withdrawal from friends
- Self-harm and suicidal thoughts or actions: they may need urgent assessment in NHS Mental Health Services
- Cannot sleep, loses their appetite, or develops a prolonged fear of being alone
- A sharp drop in work performance
- Neglects themselves
- Refusal to believe that the person has died or that the event happened
- Talks repeatedly about wanting to join the dead person. They may need urgent assessment by NHS Mental Health Services
- Difficulties become worse or new troubles persist
Most people will be able to continue their personal and work responsibilities, but that doesn’t take away from how painful this process can be.
- It can take time. Some people need extra help to recover. This is not a sign of weakness – it can be the most conscientious, hard-working and responsible people who are hardest hit
- If things aren’t getting any better (for you), talk first to family and friends or other community support. Consider using helpline or If you can, discuss how you are feeling with a colleague, team leader or a member of your senior leadership team. You may feel that you need support from your faith or community organisation or to go to your GP for professional advice. You may want to consult formal psychological support services like – you can self-refer. Remember your psychological health is just as important as your physical health
- We tend to search for meaning, particularly if someone close to us has died in sudden or traumatic circumstances, if your relationship with the deceased was difficult, or troubles were unresolved. We try to work out why the event happened. Blaming somebody else or ourselves, or feeling guilty, is mostly wrong and nearly always unhelpful in getting over these experiences, but it is often difficult to deal with these feelings on our own
- It can be helpful to say to yourself or to a colleague, 'it was not your fault' or 'this happened to you, not because of you', 'you did everything you could, most people would have done the same' or 'you would never be this hard on anyone else'. This can help to counter the tendency towards guilt and self-blame
- You may want and need a longer, more thorough psychological intervention. That is quite common in these circumstances, particularly after the crisis has passed. Do ask. You deserve it. Calling a helpline, such as Education Support can be a first step for some, and you can always call Samaritans at any time. Your line manager, Occupational Health, GP or manager should also be able to direct you to further support
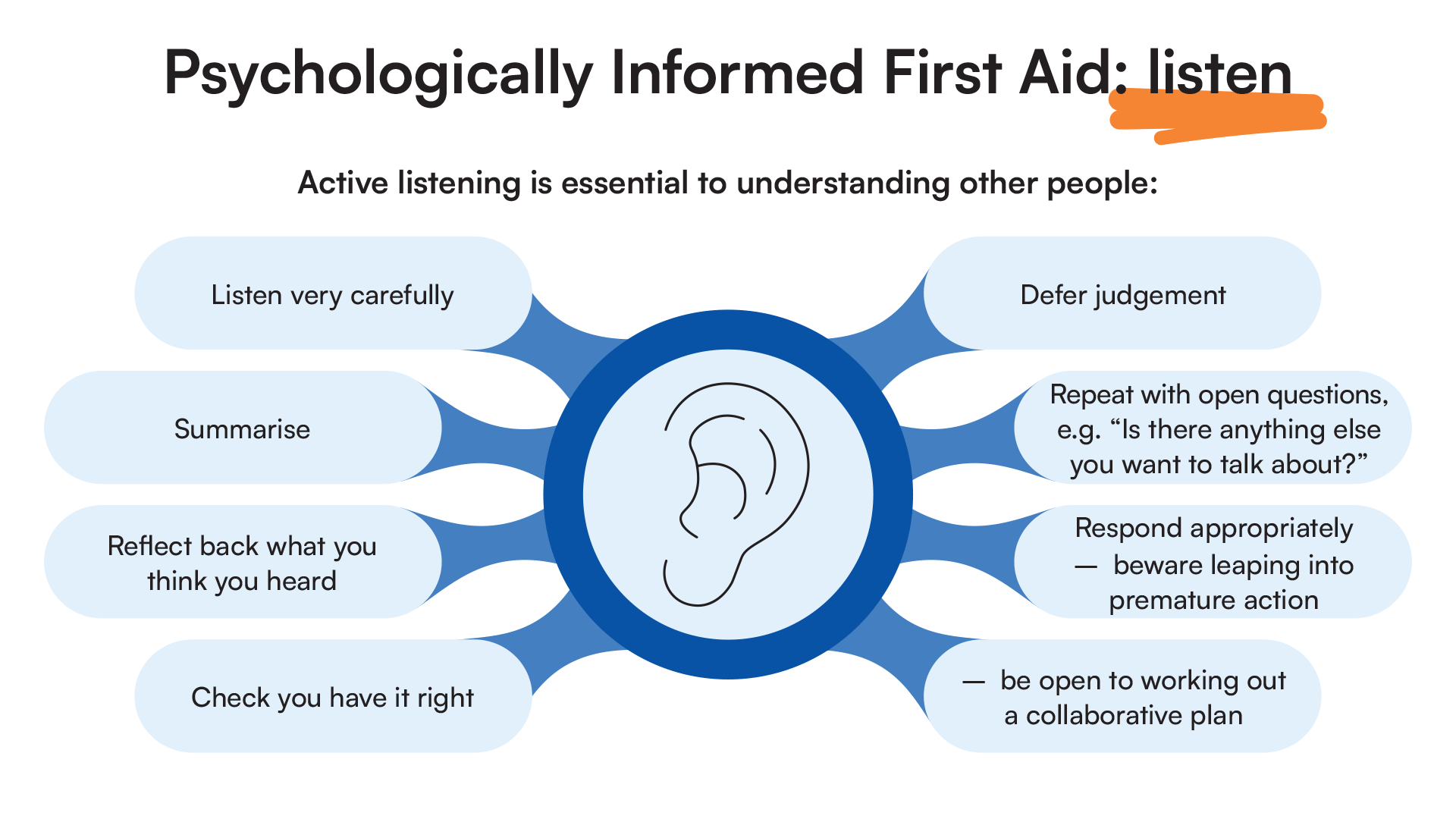
- Psychologically informed first aid for all ages illustrated here gives a framework tool to support colleagues whose mental health you may be concerned about
Further Resources
For yourself and for those in your education community
For children and young people affected by loss and death
- Anna Freud Centre - Bereavement and Loss
- Child Bereavement UK Specific information for the education sector, including a live chat Monday – Friday 9.00-5.00 and a Helpline 0800 02 888 40
- Child Bereavement UK and London Grid for Learning Managing a Sudden Death in the Community
- Cruse- variety of leaflets which may be helpful, including in Welsh language
- Government of Wales national framework for bereavement care
- Manchester Resilience Hub
- MindEd Mindfulness e-learning session
- National Suicide Prevention resources
- Winston's Wish - free online bereavement training accessible without charge after registration
- Young Minds - Grief and Loss
Wellbeing for Education Return Webinars
- Webinar 1: Describes whole School/College approaches, wellbeing and support of resilience building in the context of Covid-19
- Webinar 2: focuses on those who may need additional support with one or more of; Loss, Bereavement, Grief, Anxiety, Low Mood, Stress, Trauma in the context of Covid-19
Broader Mental Health Services
- Anna Freud Centre
- Charlie Waller Trust
- Guidance for parents and carers on supporting children and young people’s mental health and wellbeing during the coronavirus (COVID-19) pandemic
- MindEd for Families
- Royal College of Psychiatrists - information about various mental health disorders with information for patients, carers, family and friends relating to mental health problems and disorders - with downloadable free leaflets
- Young Minds
Other support groups and caring organisations you may find helpful include:
- Assist Trauma Care – Offers telephone counselling and support to individuals and families in the aftermath of trauma. Tel: 01788 551919
- Cruse – Bereavement Care – Offers counselling, advice and support throughout the UK. Tel: 0808 808 1677
- Domestic Violence Intervention Project – offers advice and support to individuals and families who have experienced domestic violence as well as to individuals who want to change their behaviour. Tel: 020 7633 9181.
- Drinkaware – offers facts, advice and support to manage drinking. Tel: 020 7766 9900
- Relate – offers relationship support for couples and families. Tel: 0300 0030396
- Samaritans – offers a 24- hour helpline for those in crisis. Tel: 116 123
- Stonewall – offers information, advice and support for gay, lesbian, bi, and trans communities. Tel: FREEPHONE 0800 0502020
Acknowledgements
The content for these tips was written and edited by Dr Raphael Kelvin and Dr Julie Greer. They draw upon the suite of tips on the MindEd Hub and input from our reference groups of healthcare and education setting experts, to whom we are most grateful.
Education Reference Group: John Dexter, John Ivens, Margaret Mulholland, Steve Rippin, Jason Turner
Wider Stakeholder Group: Sinéad Mc Brearty, Faye McGuinness, Joanna Holmes, Lisa Shostack, Mina Fazel, Andy Bell, Ray McMorrow, Sarah Hannifan, James Brown, DFE (Emma Woodshaw), Sarah Lyons, Steve Cooper
© 2022 Education Support Limited, MindEd / Royal College of Psychiatrists and Health Education
Disclaimer
This document provides general information and discussions about health and related subjects. The information and other content provided in this document, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment.
If you or any other person has a medical concern, you should consult with your healthcare provider or seek other professional medical treatment. Never disregard professional medical advice or delay in seeking it because of something that you have read in this document or in any linked materials. If you think you may have an emergency, call an appropriate source of help and support such as your doctor or emergency services immediately.
MindEd is created by a group of organisations and is funded by NHS England, the Department of Health and Social Care and the Department for Education.
© 2023 NHS England, MindEd Programme